A lot of questions start popping in the minds of the
patient and their loved ones once they hear the
doctor/nurse say, “the patient needs Surgery”. What kind
of surgery, how much will it cost, how serious it is, and
most importantly what will happen once the surgery is
over? Many family members plan to take the patient home
thinking that a loving environment can probably help them
heal faster but is it safer too?
With this article, we try to bring attention to the issues
a patient or their loved ones would suffer if they are
directly taken home post-surgery.
Why should families avoid taking patients home directly post-surgery?
Post-surgery or an ICU treatment, patients generally long to go home to their comfort zone and prefer to recuperate in the presence of their loved ones. However, it is important to understand that it may be preferable to not take a patient home directly. Patients can face various complications post-surgery/ ICU care which needs to be treated in a hospital/healthcare centre. A few such concerns can be:
- Vital signs help in monitoring the medical condition of the patient. A sudden change in vital signs calls for a rapid response system that might not be available at home easily.
- Medication management differs in a home setting. Taking the right medicine at the right time can be a difficult job. Sometimes, the medicines prescribed by the doctor might not also be available at the nearby pharmacy.
- Inotropic support like NORAD or Dopamine NTG is given to patients with cardiac conditions. The intake of such medicines is always monitored by the doctor as it may vary according to the other medicines that the patient is taking.
- Oxygen delivery management deals with providing oxygen to patients with pulmonary diseases or diseases that make breathing difficult. Small oxygen cylinders only last for a minimum amount of time and can leave the patient short of breath causing more problems.
- Continuity care: With a health professional at home it is not certain that they will stick around until the patient is well. They might have a change of shift or workplace. Due to this, the patient's family might have to bring a new nurse and explain the entire procedure of care again which can be a strenuous task.
- Doctor’s visiting hours: The doctor might not be available at all times like in a hospital. He might get stuck in surgery or due to some prior commitments cannot reach the place on time.
- Presence of a Family member in case of requirement: The healthcare provider is not familiar with the whereabouts of the house. So, one of the family members always has to be there assisting the nurse or the doctor.
- Waste management: Biomedical waste just doesn't pollute the environment but can also be of great threat to the people who might come in contact with it. Disposal of such hazardous waste is difficult at homes and can spread further infection.
- Bleeding risks in suction during Tracheostomy: A simple yet complicated procedure with many risks involved with it. Inserting the cannula, pressure on the bleeding vessels, placing of tracheostomy tubes, etc. everything needs to be done with full insight into the procedure.
- Blood transfusion is a way of adding blood to the body which cannot take place at home. The blood is given through a needle or an IV line and needs monitoring after the transfusion in a hospital setting.
Issues of the above kind are difficult to deal with at home. They need to be dealt with in a hospital or a hospital-like setting where active care can be managed and immediate response measures can be undertaken to avoid any fatalities. Only once the patient’s condition stabilizes, problems like pressure ulcers are reduced to a manageable level and probabilities of the patient collapsing become low are when the patient family should plan to shift a patient home.
Risks involved
Other than the above medical management issues, there are certainly other risks involved with taking patients home directly post-surgery/ICU care.
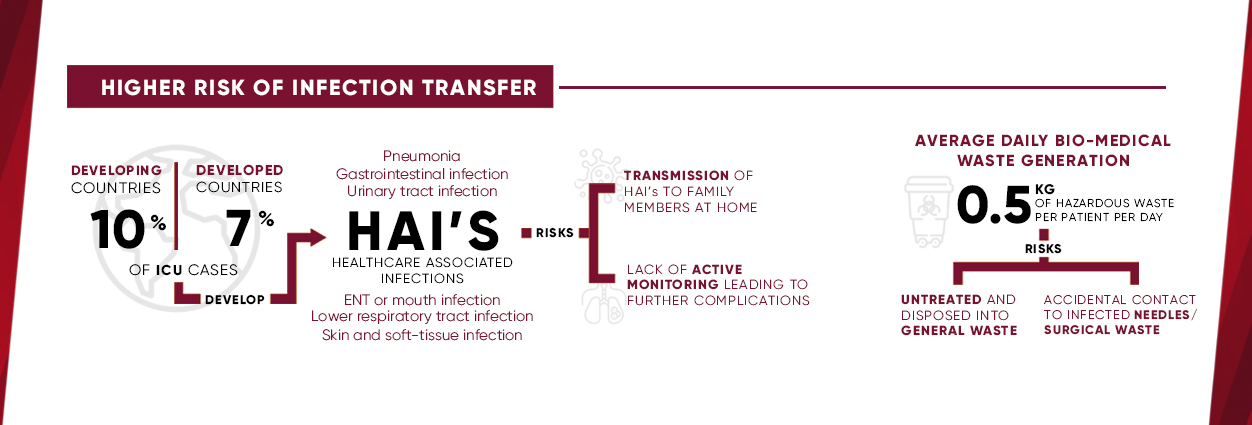
1. Risk of Infection to patients and family
members:
Due to the nature of hospitalization, patients generally
tend to develop HAI’s (Healthcare-associated infections).
Patients are most prone to these infections in ICUs.
Certain examples of the above are:
a. Pneumonia
b. Gastrointestinal Infections
c. Urinary
Tract Infections
d. ENT infections
In cases
when a patient is shifted home directly with an HAI, the
chances of transmission of these infections to other
family members are heightened. The vice versa, the
probability of transmission of an infection from family
members to the patient also increases at home.
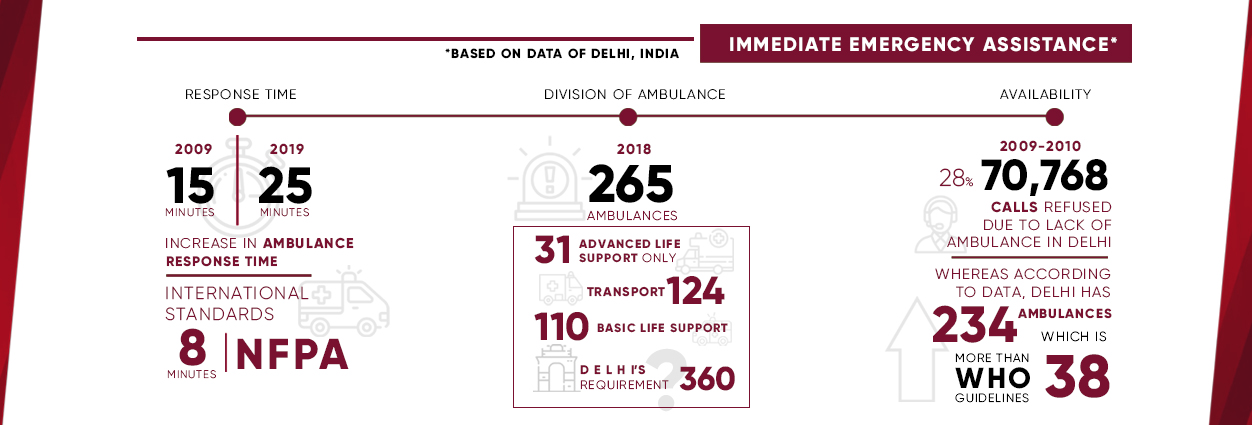
2. Lack of Immediate Emergency Assistance: With the increasing population and population density in urban areas, we are now seeing an increase in ambulance response times. Even though cities like Delhi have the required number of ambulances as per WHO guidelines, the number of Advanced life support ambulances is a meagre 11% of the total. With these trends, it becomes difficult to predict the availability of emergency services when we require them the most.
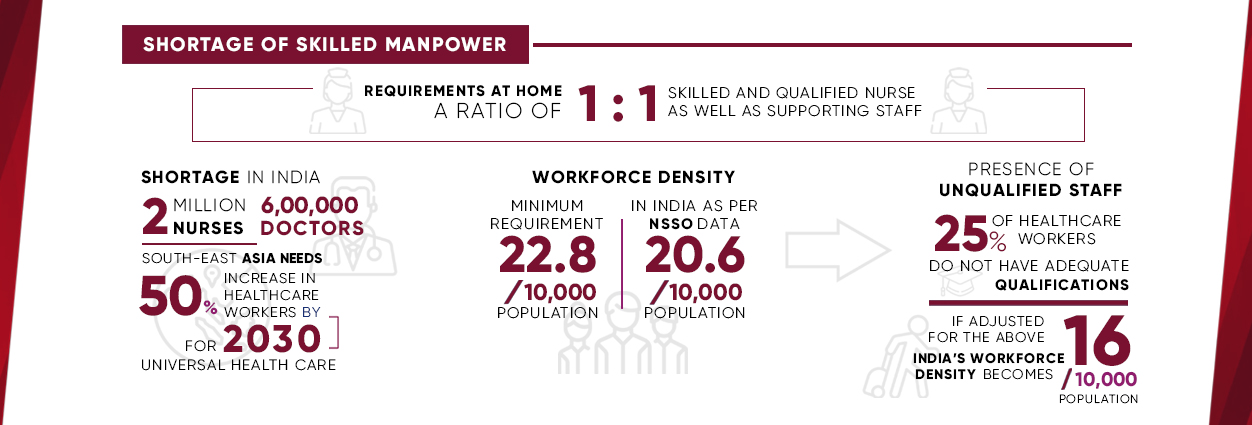
3. Skilled Nursing Care: India is facing an acute shortage of healthcare workers. To top the above shortage, about 25% of the current healthcare workers do not meet the healthcare qualifications and standards. The innate issue with patients getting treated at home is that the Patient to Nurse Ratio is 1:1. One nurse gets restricted to 1 patient management due to location constraints. In situations where patients are critical or have had recent surgery, the need for skilled nurses and paramedics is the need of the hour and when treating the patient at home, this usually ends up being a constraint.
4. Emotional and physical stress: As the patient needs extra care as soon as they are out of surgery both mentally and physically, so does the supporting family. The family has to be acceptable to the all-over a change in their comfort zone. Emotionally the family might be satisfied to have their loved ones near them but psychologically it's a stress to see them wired to so many machines. The members might also limit their mobility considering the health of the patient. Having a nurse or a doctor at all times in the house might also give a strange feeling to the family.
5. Limited Monitoring leading to increased recovery time: Many people believe that once the patient is shifted back home it is not necessary to keep a check on the vital signs until insisted by the doctor. Machines like automated external defibrillators, or AEDs, vital sign monitors, ECG monitors, etc. may not be easily accessible at home. This can be a problem as it will limit the monitoring of the patient and slower their recovery process.
Conclusion
With the growing elderly population and concerns around the quality of institutionalized care, family caregivers are demanding worthwhile solutions to provide care for their loved ones. No matter how big or small the problem is, the family or the loved one will always be there to support the patient. The real decision making starts with post-surgery discharge. To avoid heavy bills and the hospital environment the patient tends to go home directly without any extra care. But they need to be pre-prepared to face further challenges as it not only delays their recovery process but also can risk infection to their family members.
“Go Home. Go Better.”
https://www.webmd.com/healthy-aging/features/surgery-post-op#1
https://www.webmd.com/healthy-aging/features/home-self-care#3
https://factly.in/what-is-the-state-of-emergency-ambulance-services-in-india/
https://www.hindustantimes.com/delhi-news/cats-ambulance-responding-to-more-calls-but-taking-15-minutes-longer-to-reach-patients/story-aCViC12oUZpBTqtRa7MgMP.html
https://health.economictimes.indiatimes.com/news/industry/where-does-india-stand-in-the-global-home-healthcare-sector/66845982
https://www.who.int/news-room/fact-sheets/detail/health-care-waste
https://www.who.int/gpsc/country_work/gpsc_ccisc_fact_sheet_en.pdf
https://economictimes.indiatimes.com/industry/healthcare/biotech/healthcare/india-facing-shortage-of-600000-doctors-2-million-nurses-study/articleshow/68875822.cms?from=mdr
https://sabrangindia.in/article/india-facing-critical-shortage-skilled-healthcare-providers

